Intrauterine Insemination & Tubal Recannalization (IUI)
TUBAL RECANALIZATION
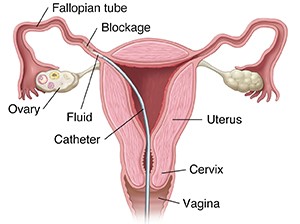
Are your tubes blocked making it hard to get pregnant? Then FALLOPIAN TUBE RECANALIZATION is just the thing for you!
Blocked fallopian tubes is a major cause of infertility for many women, especially those who had history of STDs, or endometriosis, or previous pelvic surgery. Recanalization is the medical term for “reopening.” Fallopian tube recanalization can help remove mucus or debris that is blocking one or both fallopian tubes. During the 30-minute procedure, a tiny catheter is passed into the cervix by hysteroscopy to the Fallopian tube and the blockage is cleared.
When the tubal blockage is close to the uterus, its technical success rate is 90% and is extremely effective for treating tubal obstruction. This would allow for NATURAL conception and for conceiving with IUI, without the need for IVF.
Why IUI is better than sex in order to conceive?
IUI provides 4 advantage over sex alone:
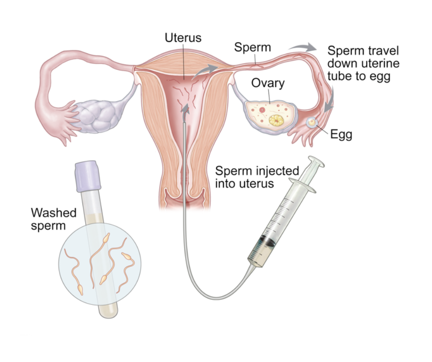
- Best sperm! In IUI, the lab will process the sperm (called sperm washing) in order to get the best quality sperm at a high concentration since only a small percentage of the sperm is viable.
- Shorter distance for the sperm to reach the egg! IUI shortens the distance the sperm needs to travel and increasing the chance of sperm reaching the egg to achieve fertilization.
- Better timing! We will monitor your ovulation closely in order to make sure that the sperm and the egg meet at the right time
- Avoid the vagina! A lot of sperm gets killed in the vagina due to the acidity of the vagina. During the IUI process, the sperm is not exposed to the vaginal acidity because they are deposited immediately inside the uterus.
You are a candidate for IUI if:
- You have at least one open fallopian tube
- You are using donor sperm (for example: Lesbian couple)
- You have irregular period/ovulation such as in PCOS
- You have unexplained infertility (infertility in which the exact cause cannot be identified)
- Sperm has mild abnormalities
- You have endometriosis (a painful inflammatory condition of the female pelvis)
- Vaginal/Cervical factor infertility (related to prior surgery such as LEEP)